What is the Cause of Keratoconus? Complete Guide
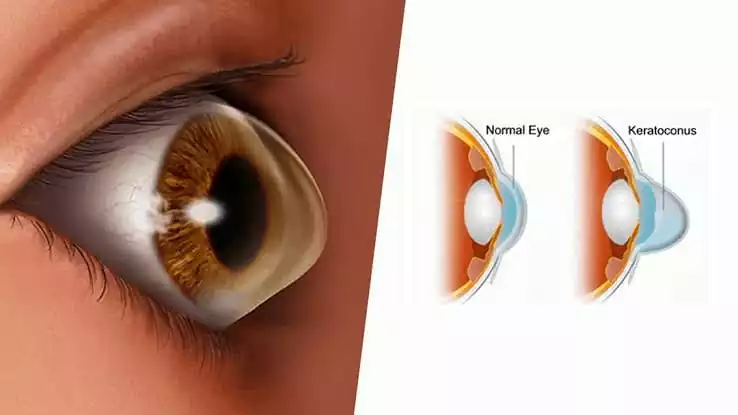
Keratoconus is a condition that affects the eye, specifically the cornea. The cornea is the clear, dome-shaped surface that covers the front of the eye. When someone has keratoconus, the cornea becomes thinner and gradually bulges outward into a cone shape. This abnormal shape can cause vision problems, which may worsen over time if not treated.
Understanding Keratoconus
Keratoconus typically begins in the teenage years and can progress into a person’s mid-thirties. The condition affects the clarity of vision, making it difficult to see things clearly. People with keratoconus often find that their eyesight changes frequently, and they may need new glasses or contact lenses often. The severity of keratoconus can vary from person to person, with some experiencing only mild symptoms while others have more significant vision problems.
What Should You Avoid if You Have Keratoconus?
The Role of Genetics
One of the primary causes of keratoconus is genetics. Research has shown that keratoconus tends to run in families. If a person has a close relative with keratoconus, they are more likely to develop the condition themselves. Scientists believe that multiple genes are involved in causing keratoconus, although the exact genes responsible have not yet been identified.
Environmental Factors
In addition to genetics, environmental factors can also contribute to the development of keratoconus. People who frequently rub their eyes are at a higher risk of developing the condition. Eye rubbing can damage the delicate tissue of the cornea, making it thinner and more likely to bulge. People with allergies, especially those who experience itchy eyes, may be more prone to rubbing their eyes, increasing their risk of keratoconus.
The Role of the Cornea
The cornea plays a crucial role in the development of keratoconus. In a healthy eye, the cornea is strong and maintains its dome shape. However, in people with keratoconus, the cornea becomes weaker over time. This weakening causes the cornea to thin and change shape, leading to the symptoms of keratoconus. The exact reason why the cornea weakens in people with keratoconus is not fully understood, but it is likely a combination of genetic and environmental factors.
How Do You Treat Keratoconus?
Other Contributing Factors
Several other factors may contribute to the development of keratoconus. People with certain medical conditions, such as Down syndrome, Ehlers-Danlos syndrome, and Marfan syndrome, have a higher risk of developing keratoconus. These conditions affect the body’s connective tissues, including the cornea, making it more likely to become thin and cone-shaped.
Hormonal Changes
Some researchers believe that hormonal changes during puberty may play a role in the development of keratoconus. Since the condition often begins during the teenage years, it is possible that the hormonal changes that occur during this time contribute to the weakening of the cornea. However, more research is needed to understand the link between hormones and keratoconus.
Early Detection and Management
Early detection of keratoconus is crucial for managing the condition and preventing severe vision problems. Regular eye exams are essential, especially for individuals with a family history of keratoconus or those who have conditions that increase their risk. Eye care professionals can use various tests to detect keratoconus, including corneal topography, which maps the shape of the cornea.
What Happens If Keratoconus Is Left Untreated?
Treatment Options
While there is no cure for keratoconus, several treatments can help manage the condition and improve vision. In the early stages, glasses or soft contact lenses may be sufficient to correct vision problems. As the condition progresses, more specialized contact lenses, such as rigid gas permeable lenses or scleral lenses, may be needed to provide clearer vision.
For people with more advanced keratoconus, procedures such as corneal cross-linking may be recommended. This treatment involves applying a special solution to the cornea and using ultraviolet light to strengthen the corneal tissue. Corneal cross-linking can help to slow or stop the progression of keratoconus, reducing the risk of further vision loss.
In severe cases, where the cornea has become significantly thin and misshapen, a corneal transplant may be necessary. During this procedure, the damaged cornea is replaced with healthy donor tissue. While a corneal transplant can restore vision, it is usually considered a last resort after other treatments have been tried.
What is the Role of an Ophthalmologist in Eye Care?
Conclusion
Keratoconus is a complex condition with multiple causes, including genetic factors, environmental influences, and possibly hormonal changes. Early detection and appropriate treatment are essential for managing keratoconus and maintaining good vision. While the condition can be challenging, advances in eye care and treatment options offer hope for people living with keratoconus. Regular eye exams and avoiding eye rubbing are simple yet effective steps that can help reduce the risk of developing keratoconus or slow its progression.
Take the First Step with Imperial Healthcare
If you or a loved one are experiencing symptoms of keratoconus or have concerns about your eye health, don’t wait. At Imperial Healthcare, our team of experienced eye specialists is here to provide you with the highest level of care. We offer advanced diagnostic tools and treatment options to help manage keratoconus and protect your vision. Schedule your consultation today and let us help you maintain clear and healthy eyesight for years to come.
Book Your Appointment Today!
Frequently Asked Questions
How is keratoconus diagnosed?
Keratoconus is diagnosed through a comprehensive eye exam, including corneal topography, which maps the shape of the cornea, and other tests to assess the cornea’s thickness and structure.
Can keratoconus be cured?
There is no cure for keratoconus, but it can be managed with treatments like specialized contact lenses, corneal cross-linking, and in severe cases, corneal transplants to improve vision and slow progression.
Who is at risk of developing keratoconus?
Individuals with a family history of keratoconus, those who frequently rub their eyes, and people with certain medical conditions affecting connective tissue are at higher risk of developing keratoconus.
What are the symptoms of keratoconus?
Symptoms of keratoconus include blurred or distorted vision, frequent changes in prescription glasses or contact lenses, and increased sensitivity to light, often worsening over time if untreated.
How can keratoconus be managed?
Keratoconus can be managed with glasses, specialized contact lenses, or treatments like corneal cross-linking. Early detection is key to slowing progression and maintaining good vision quality.