Is Keratoconus Linked to Autism?
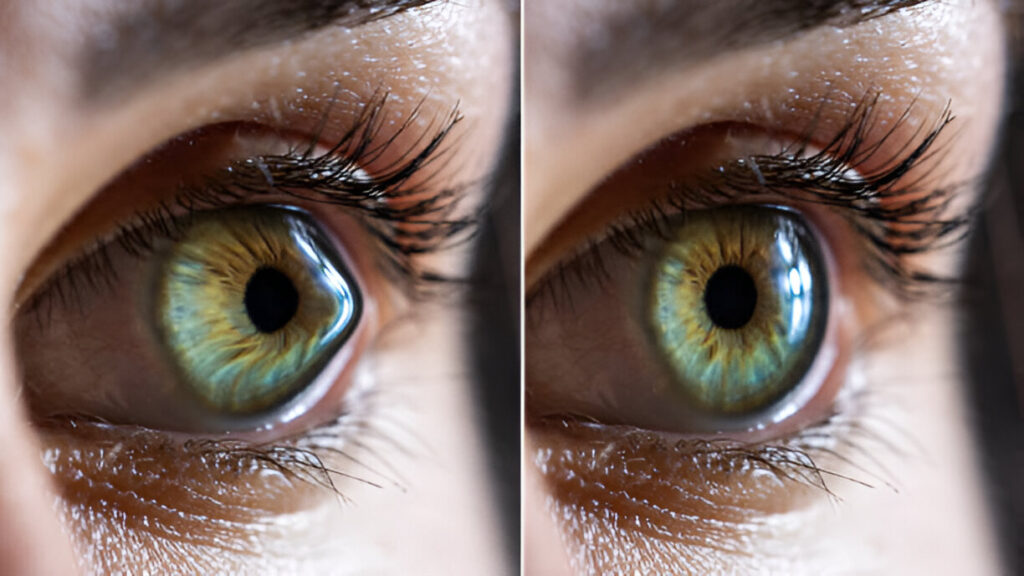
Keratoconus is a progressive eye condition where the cornea, the clear front part of the eye, thins and bulges into a cone shape. This change distorts vision and can lead to significant visual impairment. Autism Spectrum Disorder (ASD), on the other hand, is a neurodevelopmental condition that affects communication, behavior, and social interactions. Recently, there has been growing interest in whether there is a potential link between keratoconus and autism. In this article, we explore the possible connection, examining the factors that might contribute to this association.
Eye Rubbing and Its Role in Keratoconus
One of the key factors in the development and progression of keratoconus is frequent eye rubbing. Eye rubbing is more than just a habit; it can weaken the corneal structure over time, leading to the characteristic thinning seen in keratoconus. Children with autism are often observed to engage in repetitive behaviors, including eye rubbing, which raises the question of whether this could be a contributing factor in the development of keratoconus in individuals with ASD.
The Behavioural Link: Autism and Eye Rubbing
Children with ASD often exhibit repetitive motor behaviors, such as hand flapping, rocking, or eye rubbing. Eye rubbing, in particular, may be exacerbated by sensory sensitivities or allergies, which are also common in individuals with autism. The combination of repetitive eye rubbing and underlying allergic conditions could potentially accelerate the onset of keratoconus in these children. This behavioral link suggests that eye rubbing, driven by ASD symptoms, might be a significant risk factor for keratoconus.
Case Studies and Clinical Observations
Recent case reports have documented instances where children with ASD developed keratoconus, often linked to their persistent eye rubbing habits. In one case, a 14-year-old boy with autism was diagnosed with keratoconus after a noticeable decline in his visual acuity. Despite undergoing corneal cross-linking, a standard treatment to halt the progression of keratoconus, his condition worsened, likely due to ongoing eye rubbing. Behavioral interventions to reduce eye rubbing eventually helped stabilize his condition, underscoring the importance of addressing these habits early on.
The Need for Broader Research
While case studies provide valuable insights, they are not enough to establish a definitive link between keratoconus and autism. There is a clear need for broader research that includes larger population studies to determine whether individuals with ASD are indeed at higher risk for developing keratoconus. Such studies could compare the prevalence of keratoconus in autistic individuals with that in the general population, providing a clearer picture of any potential link.
How Do You Treat Keratoconus?
Genetic and Biological Factors
Another area that requires further exploration is the potential genetic or biological mechanisms that could connect keratoconus and autism. Both conditions have been linked to genetic factors, but the exact relationship between them remains unclear. Research into whether there is a shared genetic predisposition or whether other biological factors are at play could offer new insights into why some individuals with autism might be more prone to developing keratoconus.
Early Detection and Prevention Strategies
Given the potential risk of keratoconus in children with autism, early detection and prevention are crucial. Parents and caregivers should be aware of the signs of keratoconus, such as frequent eye rubbing, squinting, or complaints of blurry vision. Regular eye check-ups, particularly for children with ASD, can help detect keratoconus in its early stages, allowing for timely intervention. Behavioral management strategies, such as teaching alternative coping mechanisms for sensory sensitivities, can also reduce the risk of keratoconus progression.
What Happens If Keratoconus Is Left Untreated?
Conclusion
The possible link between keratoconus and autism is a complex and multifaceted issue that requires further investigation. While repetitive eye rubbing, a common behavior in children with autism, appears to be a significant factor in the development of keratoconus, more research is needed to fully understand this connection. By exploring genetic, biological, and behavioral aspects, we can gain a better understanding of how to prevent and manage keratoconus in individuals with ASD. Early intervention and targeted prevention strategies may be key in protecting the vision of children with autism who are at risk for this challenging condition.
As we continue to learn more about the relationship between keratoconus and autism, it is essential to focus on proactive care. Regular eye examinations, early behavioral interventions, and a better understanding of the underlying factors can make a significant difference in the lives of those affected by both conditions. The journey to uncover the full extent of the link between keratoconus and autism is ongoing, but with continued research and awareness, we can hope to improve outcomes for those at risk.
What is the Role of an Ophthalmologist in Eye Care?
Protect Your Child’s Vision with Imperial Healthcare
At Imperial Healthcare, we understand the unique needs of children with autism and the potential risks they may face, including keratoconus. Our expert team is here to provide comprehensive eye care, early detection, and personalized treatment plans to help protect your child’s vision. Don’t wait—schedule an eye examination with us today to ensure your child’s eyes are healthy and well-cared for. Trust Imperial Healthcare to deliver the care and support your family deserves.
Book Your Appointment Today!
Frequently Asked Questions
Is there a link between autism and keratoconus?
There may be a connection, particularly due to repetitive eye rubbing, common in individuals with autism, which can contribute to keratoconus development.
How is keratoconus treated?
Treatment options include corneal cross-linking, specialized contact lenses, and in advanced cases, corneal transplants.
Can keratoconus be prevented in children with autism?
Early detection, regular eye exams, and managing repetitive eye rubbing can help reduce the risk of keratoconus in children with autism.
What are the symptoms of keratoconus?
Symptoms include blurry vision, increased sensitivity to light, frequent changes in eyeglass prescriptions, and difficulty seeing at night.
At what age does keratoconus typically develop?
Keratoconus usually develops during adolescence or early adulthood, but early signs can appear in childhood.
Why is eye rubbing harmful?
Frequent eye rubbing can weaken the cornea, leading to the development or worsening of keratoconus, especially in individuals with predisposing factors like autism.