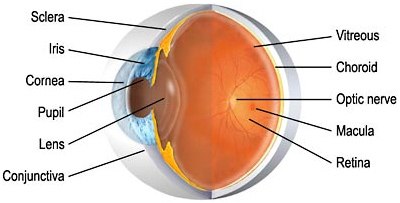
- The cornea is the clear, transparent front layer of the eye through which light passes.
- The iris gives our eyes color and it functions like the aperture on a camera, enlarging in dim light and contracting in bright light. The aperture itself is known as the pupil.
- The lens helps to focus light on the retina.
- The retina is the innermost layer of the back of the eye. This layer of light-sensitive nerve endings carries the visual impulse to the optic nerve. The macula is the central zone of the retina which provides our most central, acute vision.
- The optic nerve conducts visual impulses to the brain from the retina.
General eye examination is more than just getting your eyes checked for a lens prescription. It involves several tests to check your eyes for vision and for any eye disease.
The first comprehensive eye examination of the child should be done at 3 years unless some eye problem is noticed before that. Your ophthalmologist will check for normal 20/20 vision, lazy eye and crossed eye. If any vision problem is found the next regular eye checkup should be done as advised by your doctor. If not, the next eye checkup for the child should be done every two years. Early detection of any eye problem will help to provide timely treatment and thus will prevent deterioration of vision.
The first comprehensive eye examination of the child should be done at 3 years unless some eye problem is noticed before that. Your ophthalmologist will check for normal 20/20 vision, lazy eye and crossed eye. If any vision problem is found the next regular eye checkup should be done as advised by your doctor. If not, the next eye checkup for the child should be done every two years. Early detection of any eye problem will help to provide timely treatment and thus will prevent deterioration of vision.
- 20 to 40 years should go for general eye examination every 5 years.
- 40 to 65 years should go for it every 2 years.
- Above 65 years should go for it every year.
In case you have a family history of eye disease or vision problem or chronic disease such as diabetes that may affect vision, more frequent eye checkups would be required.
When you go for your eye examination the doctor will ask you about any vision problems you are facing or have had before and also about family history of diabetes, high blood pressure or heart disease. You should take your eyeglasses or contact lenses if using them along with you when going for the general eye examination.
General eye examination includes a number of tests that ascertain the health, function and appearance of different parts of the eye. They are:
When you go for your eye examination the doctor will ask you about any vision problems you are facing or have had before and also about family history of diabetes, high blood pressure or heart disease. You should take your eyeglasses or contact lenses if using them along with you when going for the general eye examination.
General eye examination includes a number of tests that ascertain the health, function and appearance of different parts of the eye. They are:
- Visual acuity test checks how well you can see from a distance of about 20 feet. You are asked to read aloud the letters written on a chart or screen (Snellen chart). The letters decrease in size as you read from the top line to the bottom line.
- Eye muscle test checks the function of the eye muscle used for movement of the eye. The doctor checks it by asking you to look at the pen or any other object without moving the neck when the doctor moves it in certain directions.
- Refraction test determines whether you need corrective lenses or your vision is normal. In case you need corrective lenses, it determines the prescription of lens that will give you the best possible vision. Your doctor may use computerized refractor or retinoscopy to determine your prescription for corrective lenses. In retinoscopy doctor shines a light into the eye after dilation and estimates the refractive error. Then fine adjustment for the prescription is done by making you decide which of the lenses when used in a mask like device -Phoroptor gives you the sharpest vision.
- Visual field test measures the peripheral or your side vision. It may be done using automated perimetry in which you will be asked to see into a special instrument that flashes light. If you see the light you have to press the button. It may also be determined by confrontation visual field exam in which you cover one of your eye and look at your doctor’s hand as it moves inward and outward from your visual field. You should tell your doctor when you are able to see his hand or fingers.
- Color Vision Test: In this test, the doctor will show you certain multicolored dot patterns. In case you have a certain color deficiency you will not be able to see certain patterns in those given sheets.
- Slit Lamp Examination: You are asked to sit and rest your chin and touch your forehead on the slit lamp. It magnifies the image of the eye and allows the doctor to look for any problem of the cornea, lens, iris and anterior chamber of the eye. Sometimes the doctor may stain the tear film of the eye with a fluorescein dye by using eye drop containing it or by using paper strip before examining through the slit lamp to look for cuts, foreign objects or infections of the cornea.
- Retinal examination is done to check for disease of the retina or optic nerve present at the back of the eye. The doctor will try to see the back of the eye using an ophthalmoscope or slit lamp following dilation of the pupil. The doctor may also choose to do indirect examination by using a bright light mounted on the head while each eye is kept open during examination. The eye drops used for examination will cause blurred vision and sensitivity to light for several hours even after the test. The effect will go away after a day or so.
- Glaucoma test is used to measure the internal eye pressure. It can be measured by :
Noncontact Tonometry: Here the blow of air on the eye is used to measure the eye pressure.
Applanation Tonometry: First your eye is numbed using eye drops. The eye drop also contains fluorescein to see the tear film. A gentle pressure is applied by touching the cornea using tonometer and eventually the amount of force required to flatten a part of the cornea temporarily is measured. The procedure does not hurt.
Pachymetry: After numbing the eyes an instrument is used to measure thickness of the cornea. It uses ultrasound waves to measure the same as corneal thickness is one of the significant factors that affect the intraocular pressure.
Your doctor will provide you the results of the tests within few days. In case any vision problem is detected the doctor will give you prescription for corrective glasses. However if any eye disease is detected or suspected you may be asked to go for specific eye test to confirm the initial finding.
Applanation Tonometry: First your eye is numbed using eye drops. The eye drop also contains fluorescein to see the tear film. A gentle pressure is applied by touching the cornea using tonometer and eventually the amount of force required to flatten a part of the cornea temporarily is measured. The procedure does not hurt.
Pachymetry: After numbing the eyes an instrument is used to measure thickness of the cornea. It uses ultrasound waves to measure the same as corneal thickness is one of the significant factors that affect the intraocular pressure.
Your doctor will provide you the results of the tests within few days. In case any vision problem is detected the doctor will give you prescription for corrective glasses. However if any eye disease is detected or suspected you may be asked to go for specific eye test to confirm the initial finding.
The different types of glaucoma include:
- Age over 45 years
- Family history of glaucoma
- Black racial ancestry
- Diabetes
- History of elevated intraocular pressure
- Nearsightedness (high degree of myopia), which is the inability to see distant objects clearly
- History of injury to the eye
- Use of cortisone (steroids), either in the eye or systemically (orally or injected)
- Farsightedness (hyperopia), which is seeing distant objects better than close ones.
Diabetes is a chronic disease in which your blood glucose or sugar levels are very high. Uncontrolled levels pose a risk to associated heart, kidney, and eye disorders. People with diabetes may develop three major eye problems – glaucoma, cataract, and retinopathy. The early symptom of all these disorders is blurred vision. High blood sugar causes swelling of the lens in the eye, distorting the ability to focus clearly. Retinopathy is the most common eye disease associated with diabetes, and is one of the leading causes of blindness in adults.
Diabetic retinopathy is a disease which damages the tiny blood vessels in the retina (the light-sensitive tissue at the back of the eye). Having diabetes for a long time increases the chances of developing diabetic retinopathy.
Diabetic retinopathy is a disease which damages the tiny blood vessels in the retina (the light-sensitive tissue at the back of the eye). Having diabetes for a long time increases the chances of developing diabetic retinopathy.
You chances of developing diabetic retinopathy increase with the following factors:
- Long duration and poor control of diabetes
- High cholesterol
- High blood pressure
- Pregnancy
- Tobacco
High levels of sugar in your blood from diabetes can cause damage to the blood vessels supplying the retina and loss of sight when the vessels become blocked and blood supply is cut off. In response, the eye grows new vessels, but these do not develop properly, and can leak and cause vision loss. Scar tissue can also form, pulling the retina and causing it to detach.
The early stages of the disease do not show any symptoms; but as the condition worsens you may have blurred vision, spots or dark shapes floating in your vision (floaters), lowered night vision, or temporary or permanent blindness.
Diagnosis is critical, as if it is not detected and treated early, diabetic retinopathy can eventually lead to blindness.
For Appointments
Please feel welcome to contact our friendly reception staff with any general or medical enquiry call us.
Opening Hours
Sat – Wed 10.00 AM – 7:00 PM
Thursday 10.00 AM – 2:00 PM
Friday Closed
