- Home
- Departments
- Diabetes Related Eye Conditions
Diabetes Related Eye Conditions
If you have diabetes this does not necessarily mean that your sight will be affected, but there is a higher risk. If your diabetes is well controlled then you are less likely to have problems, or they may be less serious. However, if there are complications that affect the eyes then this may result in loss of sight.
- Maculopathy is the main cause of loss vision and may occur gradually but progressively.
- It is rare for someone with maculopathy to lose all their sight.
Understanding Eye Conditions Related Diabetes
The “Understanding” series of leaflets is designed to help you, your friends and family understand a little bit more about your eye condition.
Each leaflet gives an introduction to the condition, how it can affect you, the main treatment available and how to make the most of your sight. There are details of who to contact for more information at the foot of the page.
What is diabetes?
Estimates suggest that nearly one person in twenty five in the UK is affected by mellitus, a condition which means that, due to a lack of insulin, the body cannot cope normally with sugar and other carbohydrates in the diet.
Diabetes can start in childhood, but more often begins in later life. It can cause complications which affect different parts of the body, the eye being one of them. There are two different types of diabetes mellitus:
Diabetes can start in childhood, but more often begins in later life. It can cause complications which affect different parts of the body, the eye being one of them. There are two different types of diabetes mellitus:
- Type 1 diabetes
Which can also referred to as insulin dependent diabetes mellitus (IDDM). This type of diabetes commonly occurs before the age 30 and is the result of the body producing little or no insulin. Type 1 is controlled by insulin injections.
- Type 2 diabetes
which can also be referred to as non- insulin dependent mellitus (NIDDM). This type of diabetes commonly occurs after the age of 40. in this type diabetes the body does produce come insulin, although the amount is either sufficient or the body is not able to make proper use of it. This type of diabetes is generally controlled by diet or tablets, although some people in this group will use insulin injections.
Why annual eye examinations are important
If you have diabetes this does not necessarily mean that your sight will be affected, but there is a higher risk. If your diabetes is well controlled then you are less likely to have problems, or they may be less serious. However, if there are complications that affect the eyes then this may result in loss of sight.
Most sight loss due to diabetes can be prevented, but it is vital it is diagnosed early. This can only be detected by a detailed examination of the eye. Therefore, regular, annual eye examinations are extremely important, as you may not relies there is anything wrong with your eyes until it is too late.
Most sight loss due to diabetes can be prevented, but it is vital it is diagnosed early. This can only be detected by a detailed examination of the eye. Therefore, regular, annual eye examinations are extremely important, as you may not relies there is anything wrong with your eyes until it is too late.
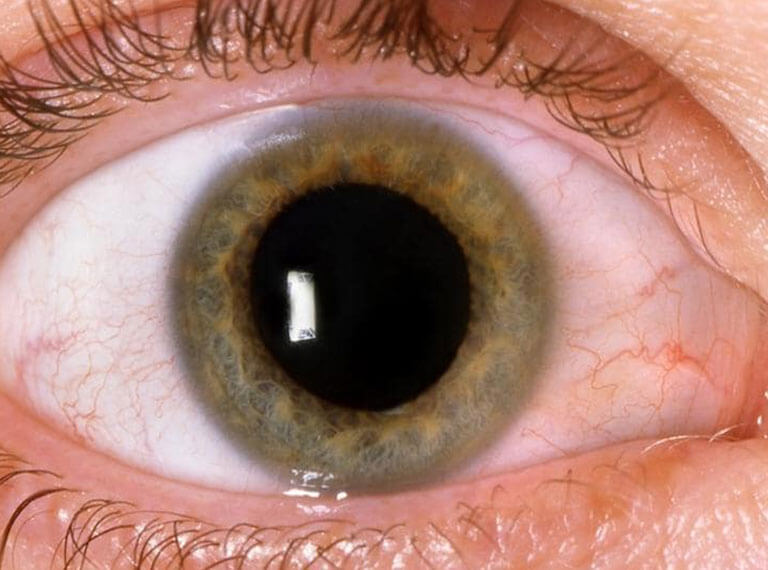
In understanding how diabetes can affect the eye, it is worth looking at how the eye works.
Your eye has a lens and an aperture (opening) at the front known as the pupil, which adjust to bring objects into focus on the retina at the back of the ye ( see diagram). The retina is made up of a delicate tissue that is sensitive to light, rather like the film in a camera. It also contains a fine network of small blood vessels.
Your eye has a lens and an aperture (opening) at the front known as the pupil, which adjust to bring objects into focus on the retina at the back of the ye ( see diagram). The retina is made up of a delicate tissue that is sensitive to light, rather like the film in a camera. It also contains a fine network of small blood vessels.
Your eye has a lens and an aperture (opening) at the front known as the pupil, which adjust to bring objects into focus on the retina at the back of the ye ( see diagram). The retina is made up of a delicate tissue that is sensitive to light, rather like the film in a camera. It also contains a fine network of small blood vessels.
Your eye has a lens and an aperture (opening) at the front known as the pupil, which adjust to bring objects into focus on the retina at the back of the ye ( see diagram). The retina is made up of a delicate tissue that is sensitive to light, rather like the film in a camera. It also contains a fine network of small blood vessels.
Diabetes can affect the eye in a number of ways. The most serious eye condition associated with diabetes involves the retina, and, more specifically, the network of blood vessels lying within it. The name of this condition is diabetic retinopathy.
Diabetic retinopathy is usually grated according to how severe it is. The three main stages are described below.
This condition is very common in people who have had diabetes for a long time. Your vision will be normal with no threat to your sight
At this stage the blood vessels in the retina are only very mildly affected, they may bulge slightly (microaneurysm) and may leak blood (haemorrhages) or fluid (exudates). The macula area of the retina mentioned earlier remains unaffected.
At this stage the blood vessels in the retina are only very mildly affected, they may bulge slightly (microaneurysm) and may leak blood (haemorrhages) or fluid (exudates). The macula area of the retina mentioned earlier remains unaffected.
With time, if the background diabetic retinopathy becomes more severe, the macula area may become involved. This is called maculopathy. I this happens, your central vision will gradually get worse. You may find it difficult to recognize people’s faces in the distance or to see details such as small print. The amount of central vision that is lost varies from person to person. However, the vision that allows you to get around at home and outside (peripheral vision) will be preserved.
Maculopathy is the main cause of loss vision and may occur gradually but progressively.
It is rare for someone with maculopathy to lose all their sight.
Maculopathy is the main cause of loss vision and may occur gradually but progressively.
It is rare for someone with maculopathy to lose all their sight.
As the eye condition progresses, it can sometimes cause the blood vessels in the retina to become blocked. If the happens then new blood vessels form in the eye. This is called proliferative diabetic retinopathy, and is nature’s way of trying to repair the damage so that retina has a new blood supply.
Unfortunately, these new blood vessels are weak. They are also in the wrong place- growing on the surface of the retina and into the vitreous gel. As result, these blood vessels can bleed very easily and cause scar tissue to form in the eye. The scarring pulls and distorts the retina. When the retina is pulled out of position this is called retinal detachment.
Proliferative retinopathy is rarer than background retinopathy.
The new blood vessels will rarely affect your vision, but their consequences, such as bleeding or retinal detachment may cause your vision to get worse. Visual loss in this case is often sudden and severe.
Your eyesight may become blurred and patchy as the bleeding obscures part of your vision.
Without treatment, total loss of vision may happen in proliferative retinopathy.
With treatment, sight –threatening diabetic problems can be prevented if caught early enough. However, laser treatment will not restore vision already lost.
Unfortunately, these new blood vessels are weak. They are also in the wrong place- growing on the surface of the retina and into the vitreous gel. As result, these blood vessels can bleed very easily and cause scar tissue to form in the eye. The scarring pulls and distorts the retina. When the retina is pulled out of position this is called retinal detachment.
Proliferative retinopathy is rarer than background retinopathy.
The new blood vessels will rarely affect your vision, but their consequences, such as bleeding or retinal detachment may cause your vision to get worse. Visual loss in this case is often sudden and severe.
Your eyesight may become blurred and patchy as the bleeding obscures part of your vision.
Without treatment, total loss of vision may happen in proliferative retinopathy.
With treatment, sight –threatening diabetic problems can be prevented if caught early enough. However, laser treatment will not restore vision already lost.
Although your vision may be good, changes can be taking place in your retina that needs treatment. Because most sight loss due to diabetic is preventable, remember.
Early diagnosis of diabetic retinopathy is vital
Have an eye examination every year
Do not wait until your vision has deteriorated to have an eye test
The importance of early treatment of diabetic retinopathy cannot be stresses enough
Eye examinations are free for people with diabetic.
Your family doctor, diabetologist or optometrist can examine your eyes for diabetic retinopathy. In some cases photographs of the retina are used to detect abnormalities without any other form of test. If a problem is found you will be referred to a consultant ophthalmologist (eye specialist) at a hospital eye clinic.
Remember, however, that if your vision is getting worse, this does not necessarily mean you have diabetic retinopathy. It may simply be a problem that can be corrected with glasses.
Early diagnosis of diabetic retinopathy is vital
Have an eye examination every year
Do not wait until your vision has deteriorated to have an eye test
The importance of early treatment of diabetic retinopathy cannot be stresses enough
Eye examinations are free for people with diabetic.
Your family doctor, diabetologist or optometrist can examine your eyes for diabetic retinopathy. In some cases photographs of the retina are used to detect abnormalities without any other form of test. If a problem is found you will be referred to a consultant ophthalmologist (eye specialist) at a hospital eye clinic.
Remember, however, that if your vision is getting worse, this does not necessarily mean you have diabetic retinopathy. It may simply be a problem that can be corrected with glasses.
Most sight-threatening problems caused by diabetic retinopathy can be managed by laser treatment if it is given early enough. It is important to realise, however, that laser treatment can only preserve the sight you have- not make it better. The laser, a beam of high intensity light, can be focused with extreme precision so that the blood vessels that are leaking fluid into the retina can be sealed.
If new blood vessels are growing, more extensive laser treatment has to be carried out.
If new blood vessels are growing, more extensive laser treatment has to be carried out.
Treatment is normally carried out in an outpatient clinic and you usually do not have to stay in hospital. Eye drops are used to enlarge the pupils so that the eye specialist can look into your eye. The eye is then numbed with drops and a small contact lens is put onto your eye to stop it blinking. During the treatment you will be asked to move your eyes in certain directions but this can easily be done with the contact lens in place.
The treatment for sealing blood vessels does not usually cause discomfort. However, the treatment to remove new vessels can be a bit uncomfortable, so you may need a pain- relieving tablet at the same time as the eye drops.
There is further pain relief available and so remember:
Do not be afraid to tell the eye specialist if the treatment is hurting
Do not be afraid to tell the eye specialist if you have found a previous session of laser treatment distressing.
There is further pain relief available and so remember:
Do not be afraid to tell the eye specialist if the treatment is hurting
Do not be afraid to tell the eye specialist if you have found a previous session of laser treatment distressing.
No treatment is possible without some side effects, but the risks of laser treatment are far less than the risks of not having laser treatment.
The treatment for sealing blood vessels has few side effects, although the laser is very bright and causes a temporary reduction of sight which may last an hour or two after the treatment; you may also lose a little central vision or notice the after-effects of the laser as small black spots in your vision.
It is quite common to lose some vision to the sides (peripheral vision) and this may affect your ability to drive safely. If you have had laser treatment for diabetic retinopathy you are required to inform the Driver and Vehicle Licensing Agency (DVLA- see useful contact details) who may request that you have your peripheral vision tested.
Night and colour vision may also be affected.
Occasionally your central vision may not be as good as before so that, for example, print is not as easy to see (this is usually temporary, but sometimes does not improve).
Laser treatment to remove new blood vessels is more complicated.
If you do have any concerns about the side effects of treatment you should discuss them with your eye specialist.
The treatment for sealing blood vessels has few side effects, although the laser is very bright and causes a temporary reduction of sight which may last an hour or two after the treatment; you may also lose a little central vision or notice the after-effects of the laser as small black spots in your vision.
It is quite common to lose some vision to the sides (peripheral vision) and this may affect your ability to drive safely. If you have had laser treatment for diabetic retinopathy you are required to inform the Driver and Vehicle Licensing Agency (DVLA- see useful contact details) who may request that you have your peripheral vision tested.
Night and colour vision may also be affected.
Occasionally your central vision may not be as good as before so that, for example, print is not as easy to see (this is usually temporary, but sometimes does not improve).
Laser treatment to remove new blood vessels is more complicated.
If you do have any concerns about the side effects of treatment you should discuss them with your eye specialist.
After lengthy treatment, most people develop a headache and so a headache can be taken for this. However, if the pain is severe, or if your eyesight gets worse, you should contact your eye specialist immediately. If this is not possible, go straight to the hospital casualty department.
If your eye condition becomes more severe, causing retinal detachment and scar tissue, or if the vitreous becomes cloudy due to recurrent bleeding, it may be possible to perform an operation called a vitrectomy. This will involve the vitreous being removed and replaced with a clear solution. It is a highly specialized operation and you should discuss the various options with your eye specialist.
Research is continuing into diabeyes0related eye conditions, and their treatment is constantly improving.
If your eye condition becomes more severe, causing retinal detachment and scar tissue, or if the vitreous becomes cloudy due to recurrent bleeding, it may be possible to perform an operation called a vitrectomy. This will involve the vitreous being removed and replaced with a clear solution. It is a highly specialized operation and you should discuss the various options with your eye specialist.
Research is continuing into diabeyes0related eye conditions, and their treatment is constantly improving.
Much can be done to help you use your remaining vision as fully as possible. You should ask your eye specialist or optometrist about low vision aids. Alternatively, you could contact the RINB helpline on 0845 766 9999 or visit the RNIB low vision website at www.rnib.org.uk/lowvision for more information about low vision services in your area.
If you vision is impaired, it is also worth registering as partially sighted or blind through your eye specialist. This opens the door to expert help and financial benefits.
If you vision is impaired, it is also worth registering as partially sighted or blind through your eye specialist. This opens the door to expert help and financial benefits.
This may occur as one of the first symptoms of diabetes although it may also occur at any time when your diabetes is not well controlled. It is due to a swelling of the lens of the eye and will clear without treatment soon after the diabetes is brought under control again.
A cataract is a clouding of the lens of the eye, which causes the vision to become blurred or dim because light cannot pass through the clouded lens to the back of the eye, this is a very common eye condition that develops as people get older but someone with diabetes may develop cataracts at an earlier age than someone without diabetes. The treatment for cataracts involves an operation to remove the cloudy lens, which is usually then replaced by a plastic, lens helping the eye to focus properly once again.
Important points to remember
- Most sight-threatening diabetic problems can be managed by laser treatment if it is given early enough
- Early diagnosis of diabetic retinopathy is vital
- Have an eye examination every year
- Do not wait until your vision has deteriorated to have an eye test
- Do not be afraid to ask questions or express fears about your treatment.
Meet Our Doctors
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries. Doctors will be available from 8 am : 12 am , kindly call to confirm your Appointment.
For Appointments
Please feel welcome to contact our friendly reception staff with any general or medical enquiry call us.
Opening Hours
Sat – Wed
10.00 AM – 7:00 PM
Thursday
10.00 AM – 2:00 PM
Friday
Closed




